In the first blog post in this series we identified over 40 potential sources of error when a syringe pump delivers a dose, all of which we considered when designing our new infusion pump for laboratory animal research. In this second post we will focus on the interface between the pump and the operator.
Potential sources of error in delivering a dose from a syringe pump
|
Operator
|
Data input error
|
Entered incorrect flow rate |
| Entered incorrect dose volume or time | ||
| Selected wrong units | ||
| Selected wrong syringe from lookup table | ||
| Entered wrong syringe ID for custom syringe | ||
| Did not start pump on time | ||
| Unintentionally stopped pump | ||
| Set pump to withdraw instead of infuse | ||
| Dislodged syringe | ||
|
Pump
|
Not moving pusher block/arm at expected rate
|
Motor speed variability* |
| Lead screw pitch tolerance* | ||
| Thread gap when engaging lead screw | ||
| Clutch not engaged/riding on top of lead screw | ||
| Pump components compressing or deflecting* | ||
| Pulsatile flow timing error* | ||
| Software error | ||
| Power failure - power outage | ||
| Power failure - cord disconnected | ||
| Power failure - battery dies | ||
| Faulty occlusion or other alarm | ||
|
Pusher moving correctly but not moving plunger at expected rate
|
Gap between pusher and syringe | |
| Syringe not perpendicular to pusher | ||
| Syringe siphoning | ||
|
Syringe
|
Inner diameter variability
|
Manufacturing variability* |
| Variability in design | ||
| Expansion/contraction due to temperature* | ||
| Expansion due to pressure* | ||
| Syringe plunger compression* | ||
| Syringe plunger sticks | ||
|
Infusion set and catheter
|
Air in line
|
Bubbles not cleared |
| Line not primed | ||
| Air permeating through tubing | ||
| Air coming out of solution | ||
| Expansion of infusion set* | ||
|
Occlusion
|
Blockage/clot | |
| Kink | ||
| Clamp not opened | ||
| ID restriction too great for given flow rate | ||
|
Leak
|
Puncture | |
| Loose connection | ||
| Rupture under pressure | ||
| Evaporation | ||
| Laminar flow* | ||
For an example of how critical the user interface can be, consider the case of the Alaris SE pump, a hospital pump that had an occasional problem with key bounce: you would press a button once and it might register it twice. This is a common problem with certain types of mechanical buttons; however, if you were setting the flow rate and you didn’t notice the error you might infuse 11 mL/hr instead of 1mL/hr. In 2006, federal agents showed up at the manufacturer and seized all the devices in production. Over 140,000 pumps were recalled.
Syringe Pump User Interfaces (Ease of Use)
While the FDA is not concerned with laboratory pumps, errors caused by a user interface that is confusing or overly complex can harm animals and ruin a study. Syringe pumps are relatively unique among electronic devices in that designs that are decades old are still in use, so there are a wide range of interfaces based on the technology that was available at the time the pump was designed.
|
Pump |
Interface Type |
How to Deliver 1mL over 30 min with BD 3mL syringe |
|
Med Associates PHM-210
|
|
|
|
New Era NE-1000
|
|
|
|
Baxter AS50 / SAI 3D
|
|
|
|
OrchesTA™ Model 100
|
|
|
|
Harvard Apparatus 11 Elite
|
|
|
|
Instech Model 400
|
|
|
Syringe Detection
Syringe pumps are only accurate if the inner diameter of the syringe is correctly used to calculate flow rate. Old Harvard Apparatus and New Era pumps require you to know and enter the syringe diameter in mm yourself. If the diameter you enter is incorrect, your flow rate will be incorrect.
In a real example, for many years Harvard Apparatus reported the inner diameter of the BD 1mL plastic syringe as 4.78mm. Somewhere along the way, perhaps due to a manufacturing revision by BD, it changed to 4.699mm. If you are still using the old figure, on average your flow rate will be 3.4% lower than what you have entered on the pump.
Newer laboratory pumps have syringe libraries with the inner diameters programmed in the pump. They should display the inner diameter as well as the syringe size so that you can verify the value. However, there is nothing preventing you from selecting a different syringe from the one you are using, which will likely lead to a large error in flow rate. Note the message on the Harvard 11 Elite screen: “Make sure to select the right syringe.”
Manufacturers of clinical pumps cannot tolerate this flow rate error risk, so those pumps have sensors that measure the outer diameter of the syringe to confirm or in some cases auto-detect the installed syringe. These sensors have the added benefit of being able to detect if a syringe has become dislodged, another potential cause of a large dose error. The downside of a clinical pump is that if you want to use a syringe that is not in the library, you are out of luck.
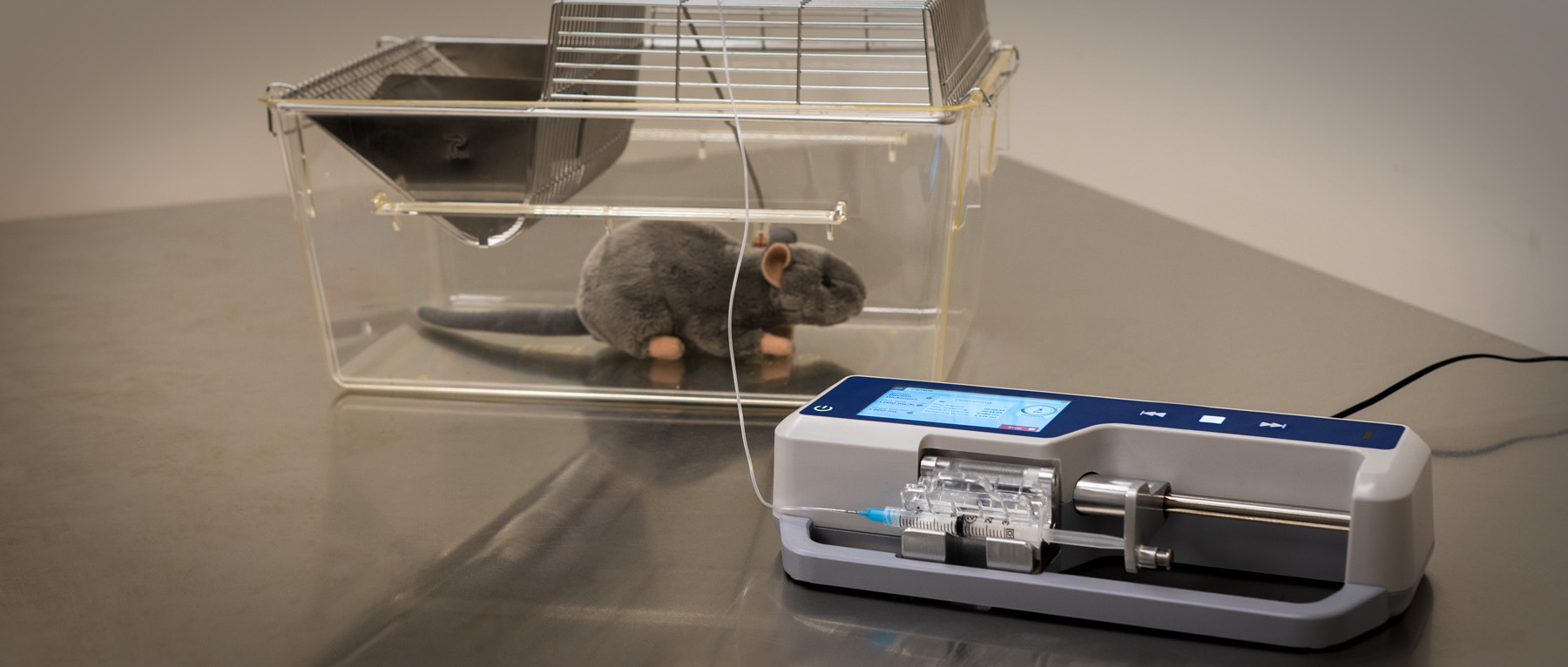
The new Instech model 400 pump is the first laboratory pump with syringe detection. It also allows you to enter a custom syringe if yours is not in the library - the best of both worlds. Furthermore, the shape of the pump is such that syringes do not extend past the frame, offering protection against dislodgment.

Infuse vs Infuse/Withdraw
Many industrial syringe pumps have the ability to withdraw as well as infuse. In most cases this is a simple button which could be pressed accidentally. Certain older Harvard Apparatus model 11 pumps even have a toggle switch on the back of the pump; if it is set to withdraw you cannot tell from the front.

This blog series is about accuracy, and withdrawing instead of infusing creates a ridiculous -200% flow rate error, but the real issue here is animal safety. Blood will fill the catheter and clot; the animal will be lost if the mistake is not caught quickly. For animal welfare, our recommendation is that pumps that have the ability to withdraw should never be used in animal infusion studies.
In summary, do not discount the user interface as a significant factor in a pump's ability to deliver accurate doses in real world situations. Stay tuned for our next post where we will look at a syringe pump’s ability to infuse accurately when pumping at the low end of rates used in animal studies.